Four specialists from private hospitals defend deductibles/copay in the Base MHIT plan as cost-sharing to discourage “unnecessary” utilisation of health care. Base MHIT is meant to establish a basic floor of protection against catastrophic medical bills.
The Galen Centre for Health and Social Policy’s critique of Malaysia’s proposed Base Medical and Health Insurance/Takaful (MHIT) Plan in a CodeBlue article (Base MHIT Plan Shifts Costs To Patients Without Addressing Medical Inflation Causes: Galen Centre) and a subsequent FMT article (Base MHIT plan not competitive or meaningful enough, says think tank) raises important concerns that merit serious consideration.
However, a more nuanced examination reveals that their analysis overlooks the plan’s strategic positioning within Malaysia’s broader health care reform journey.
Every strategy has its pros and cons, but we truly believe the MHIT base plan is a value proposition that far outweighs any criticisms.
The Base MHIT plan is primarily designed for use at private hospitals in Malaysia, specifically targeting lower- and mid-tier private health care facilities. Public hospitals will still remain the safety net for all citizens.
The MHIT plan, introduced under Malaysia’s Reset strategy, aims to enhance health care affordability, reduce reliance on cash, and provide a sustainable alternative to rising premiums.
A journey of a thousand miles begins with a single step, and the Base MHIT plan represents precisely that essential first step toward sustainable universal health coverage (UHC). This article will systematically address our concerns while positioning the plan within Malaysia’s health care evolution.
On Cost-Shifting and Affordability Concerns
Galen Centre’s statement that the plan risks “creating a false sense of security, widening inequities in access to care, and shifting costs back onto patients, especially households already strained by rising living costs” may not necessarily be true.
The Base MHIT plan is fundamentally designed to establish a basic floor of protection against catastrophic medical bills. The deductibles and co-payments are essential cost-sharing mechanisms that discourage unnecessary utilisation, encourage responsible use of health care resources, and help keep base premiums more affordable for the wider population.
The goal is to prevent financial ruin from major health events, not to cover every single ringgit of expense. This structure is a prudent first step towards a broader social health insurance system.
The characterisation of deductibles and co-payments as mere “cost-shifting” fundamentally misapprehends the principles of insurance design and social solidarity. You cannot have your cake and eat it too.
Universal, comprehensive coverage with minimal personal contribution is economically unsustainable without massive taxation increases. The Base MHIT plan utilises carefully calibrated cost-sharing mechanisms not to burden patients, but to create a responsible consumption model that preserves the system for those who need it most.
The tiered deductible structure (RM500 for basic Standard, RM10,000-15,000 for Standard-Plus) serves as a sophisticated filtering mechanism. It distinguishes between routine health care expenses – which the public system and personal savings should appropriately handle – and catastrophic health expenditures that can bankrupt families.
This approach follows the wisdom that a stitch in time saves nine; by encouraging appropriate utilisation patterns from the outset, the plan prevents the systemic overuse that has bankrupted health care systems worldwide.
Regarding affordability for senior citizens, actuarial fairness necessitates higher premiums for higher-risk groups. However, this design creates the architectural framework into which targeted subsidies can be precisely administered.
The plan doesn’t preclude subsidies; it enables them to be directed efficiently to those most in need, rather than diluted across all beneficiaries regardless of financial circumstances.
Don’t throw the baby out with the bathwater. While the Galen Centre correctly identifies implementation risks, abandoning the structural reform because of adjustable parameters like deductible levels would sacrifice transformative potential for fixable details.
On Medical Inflation and Systemic Drivers
On Galen Centre’s statement that the plan fails to address “weak or absent regulation of pricing, limited disclosure of fees, variation in clinical practice, rising costs of medical consumables, technology and expertise”:
This critique commits a categorical error by demanding that a financing mechanism solve market structure problems. The Base MHIT plan represents the first Phase of what must necessarily be a multi-phase reform.
First things first – establishing a standardised, large-scale purchasing entity fundamentally changes the dynamics of health care negotiations.
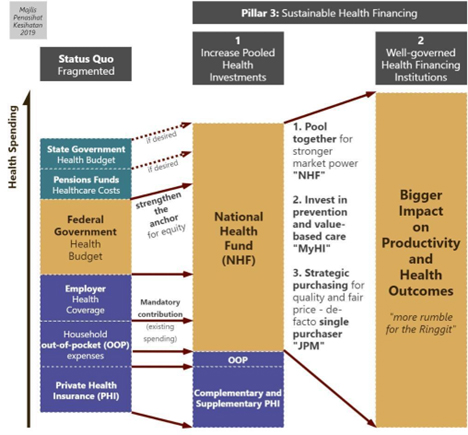
History teaches that strategic purchasing power precedes effective cost control. The establishment of the Base MHIT creates what economists call a “countervailing power” against provider monopolies.
Once millions of Malaysians are enrolled in standardised plans, the newly created purchasing entity will possess the leverage to negotiate transparent fee schedules, standardise clinical pathways, establish technology assessment protocols and demand price transparency.
The Galen Centre’s approach puts the cart before the horse. Without first creating this organised and strategic purchasing mechanism, any attempts at price regulation would lack enforcement leverage and likely fail. The plan strategically builds the foundation for precisely the reforms the Galen Centre advocates.
Malaysia cannot simultaneously solve decades of unregulated health care inflation and establish UHC. The Base MHIT plants the necessary tree whose shade will eventually cool the entire health care landscape.
On Network Limitations And Geographic Inequity
On Galen Centre’s statement: “Malaysians should not be penalized through higher co-payments simply because the network does not include a suitable facility near them… This raises concerns of unequal access.”
The tiered network design represents not a creation of inequity, but a strategic intervention into existing inequities. Where there’s smoke, there’s fire – the geographic disparities in health care access predates the MHIT proposal by decades.
The plan acknowledges this reality and creates intelligent incentives to gradually reshape provider distribution.
The tiered structure incentivises using in-network facilities, which agree to negotiated rates and standards. The challenge of rural access is a pre-existing systemic issue across all of health care, not one created by the MHIT.
The plan must start with a viable network; its success and expansion can drive investment and improvements in health care infrastructure in underserved regions over time. Public hospitals still remain the safety net.
The 20 per cent co-payment for out-of-network utilisation serves three vital functions:
- It prevents the “empty network” problem by ensuring sufficient patient volume for participating providers
- It creates market signals that encourage private health care investment in underserved regions
- It preserves the public system’s role as the universal geographic safety net
Moreover, this design consciously avoids the fatal flaw of many health reforms: promising what cannot be delivered.
By transparently acknowledging network limitations upfront, the plan builds trust through honesty rather than disillusionment through overpromising. The public health care system remains, as it should, the guaranteed provider of last resort regardless of location.
Remember: Rome wasn’t built in a day. The geographic distribution of private health care facilities represents decades of market-driven development.
The Base MHIT provides the economic incentives to gradually but systematically redirect this development toward national needs rather than purely profit-maximising locations.
This letter was written by the following:
- Dr Rajeentheran Suntheralingam, Urologist, Damansara Specialist Hospital (DSH)
- Dr Musa Mohd Nordin, Paediatrician, DSH
- Dr Ahmad Faizal Mohd Perdaus, Respirologist, DSH
- Dr Sng Kim Hock, Neurologist, Pantai Medical Centre (PMC)
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.
Published in CodeBlue: https://codeblue.galencentre.org/2026/01/rebuttal-to-galen-centres-critique-of-base-mhit-plan-part-1-dr-rajeentheran-suntheralingam-dr-musa-mohd-nordin-dr-ahmad-faizal-mohd-perdaus-dr-sng-kim-hock/